Introduction - Diffuse large B-cell lymphoma (DLBCL) is a frequent and aggressive lymphoma. First line of treatment associates an anti-CD20 immunotherapy with an anthracycline-based chemotherapy (R-CHOP). After this treatment, 30% of patients present primary refractory disease or early relapse within two years (R/R DLBCL). At date, CAR-T cells improve the prognosis of patients with R/R DLBCL compared with high-dose chemotherapy followed by autologous stem-cell transplant. However, predicting this failure remains a challenge at time of diagnosis. Current standard tools as the R-IPI score have many weaknesses, particularly for patients most at risk. A multitude of clinical, biological and PET data are available and could help to precise R/R DLBCL probability. In this study, we propose a new strategy based on machine learning and exploitation of a large dataset to early detect patients with high risk of R/R DLBCL at diagnosis.
Material and methods - Between August 2012 and November 2021, we retrospectively collected a cohort of 218 patients with DLBCL receiving first-line treatment R-CHOP. Twenty-two parameters were evaluated for each patient, including well-known predictive factors such as R-IPI components, but also advanced metabolic parameters (SUVmax, total metabolic tumor volume (TMTV), total lesion glycolysis (TLG) and Dmax), as well as pathological and biological features. We used supervised machine learning (ML) to build a multidimensional model to predict POD24, which is defined by primary refractory disease or relapse within two years. Conventional binomial logistic regression was also performed to create a conventional predictive model. In parallel, a group of three hematologists was asked to generate a consensus about POD24 occurrence using Delphi method.
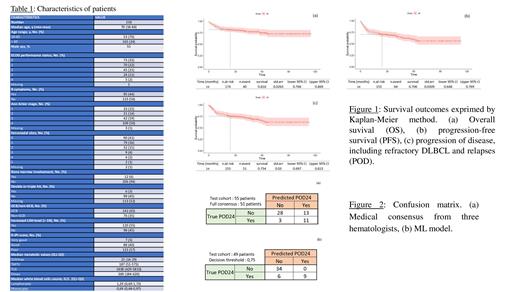
Results - Median age was 70 years. With a median follow up of 46 months, complete response rate was 87% and overall response rate was 89%. Overall survival and progression-free survival were respectively 81.6 % (95%CI 76.6 - 86.9) and 70.6 % (95%CI 64.8 - 76.9) at 24 months. POD24 event occurred in 23,5 % of patients. Performance status, Ann-Arbor staging, number of extranodal sites, medullar infiltration, TMTV, TLG, Dmax, lymphocytes and LDH showed significant predictability of POD24 when considered in univariate analysis. We used forward selection of variables to build a conventional predictive model including LDH, lymphocytes and Dmax. Area under the ROC curve was 0,72. Secondly, a ML model was trained on 147 patients and was applied on a test cohort with 49 remaining patients. Prediction accuracy was 89.7% and area under the ROC curve was 0,91. Decision threshold was raised to 0.75 cut-off, allowing to predict 60% of POD24 with 100% specificity. The four predominant variables in the model were Dmax, hepatic SUV, LDH and monocytes. Additionally, experts were confronted to 55 patients randomly sampled from the cohort, 14 (25%) of whom showed POD24. Prediction accuracy was 71% and area under the ROC curve was 0,73. Seventy-nine percents of POD24 was predicted by experts, with 68% specificity.
Conclusion - We present a ML model that was built to predict POD24 and then R/R situations in DLBCL patients. It showed great accuracy with high specificity rate. In new immunotherapies and CAR-T cells era, this proof-of-concept study highlights the fact that ML models could be a helpful to decide on first-line strategies for DLBCL patients. Larger multicentric study is necessary to confirm and validate this model for clinical use.
Disclosures
Ghesquieres:Gilead, Roche: Consultancy; Gilead, Roche, Bristol Myers Squibb, AbbVie, Novartis: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal